Anatomy/Muscular System
The muscular system is a topic of the event Anatomy for the 2020 competition, along with the integumentary system and the skeletal system.
For the muscular system you will need to know:
- The anatomy of skeletal muscle, cardiac muscle, and smooth muscle
- The roles of skeletal muscle, cardiac muscle, and smooth muscle in the body
- Skeletal muscle fibers, different types of skeletal muscle fibers, and their functions
- Skeletal muscular contraction
- The neuromuscular junction, the role of the nervous system in muscle function, and muscle sensory systems
- Musculoskeletal interactions
- How to identify the major skeletal muscles, as well as their origins, insertions, and functions
- The effects of exercise and aging on the muscular system.
- Several homeostatic imbalances affecting the muscular system
| Competition Level | Health Concepts |
|---|---|
| Regional/State | The interaction of the skeletal and muscular systems to allow movement
Muscle fibers - the cellular and gross anatomy of skeletal muscle, cardiac muscle & smooth muscle Physiology of the skeletal muscle contraction system and the neuromuscular junction How the skeletal muscles move bone, maintain posture, and produce heat Skeletal muscle actions – origin, insertion, interactions of different muscles Location and identification, including origin, insertion, and function, of the major skeletal muscles of the body listed on the 2020 Science Olympiad Major Skeletal Muscle List Exercise and aging effects on the cellular and gross anatomical structures of the muscular system Muscle and tendon injuries and their prevention (i.e., strains and sprains) The diseases on each level from the cell to the whole person as listed: Poliomyelitis, Muscular Dystrophies, Myasthenia gravis, tetanus, myositis |
| National | Kinds of muscle contraction
Classes of muscle fibers and their functions Cardiac and smooth muscle roles in the body Role of the nervous system in muscle function Muscle sensory systems (e.g., spindles and Golgi tendon organs) Additional diseases: Carpal Tunnel Syndrome, Botulism, Fibromyalgia, and Chronic fatigue syndrome Treatments and/or prevention for all conditions listed above (drugs, surgery, etc.) |
Muscles and Muscle Tissue
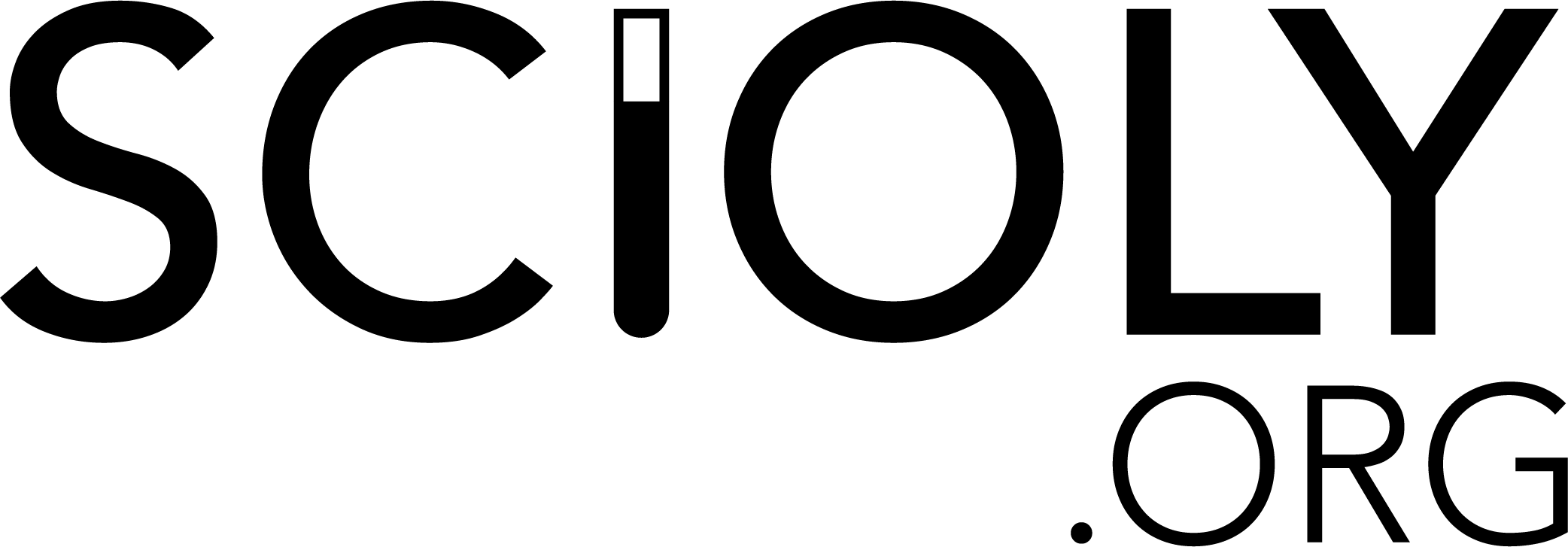
The three types of muscle tissue are skeletal muscle, cardiac muscle, and smooth muscle. Both skeletal and smooth muscle cells are elongated. For this reason, they are called muscle fibers.
- Skeletal muscles attach to the skeleton and cover it. Skeletal muscle fibers are the longest muscle fibers and they are striated. Skeletal muscles are called voluntary muscles because they are the only type of muscle subject to conscious control. Their function is mainly to give the body its mobility.
- Cardiac muscles are only found in the heart, where it constitutes the walls of the heart. Cardiac muscle cells (not fibers, cells) are also striated, but not elongated. Cardiac muscle can contract without stimulation, but it is involuntary because we do not have conscious control over our hearts. The nervous system is responsible for changes in the heartbeat.
- Smooth muscles can be found in the walls of hollow visceral organs. These organs include the stomach, bladder, and respiratory passages. It functions to force substances, especially fluids, throughout channels in the body. Smooth muscle fibers are elongated, but not striated. It is involuntary as you have no conscious control over its actions.
Muscle tissues have four special characteristics that distinguish them from other tissues.
- One characteristic that muscles have is excitability, or responsiveness, which is the ability to receive stimuli and respond to them. When muscles are stimulated by neurotransmitters, they respond by generating electrical impulses that cause their cells to contract.
- This leads to the next characteristic, contractility. Contractility is the ability for a cell to shorten in response to stimuli. This characteristic is completely unique to muscle tissues.
- Another characteristic that muscle tissues have is extensibility. This is the ability to extend or stretch. When muscles are relaxed, they can stretch beyond resting length.
- When muscles stretch beyond their resting length, they must be able to recoil in order to resume its resting length. The ability to do so is called elasticity.
Muscles serve many purposes in the body, though they have four main functions.
- Muscles are responsible for producing movements. Skeletal muscles are responsible for locomotion and manipulation. Cardiac muscles pump blood throughout your body. Smooth muscles help squeeze substances through tracts in the body.
- Muscles give the body the ability to maintain posture. Our muscles are constantly making tiny movements one after another to counteract the forces being applied to your body; for example, gravity.
- Muscles assist bones, ligaments, and tendons in stabilizing joints.
- Muscles are also responsible for generating heat. Skeletal muscles account for at least 40% of the body’s mass, making them responsible for generating heat. This helps maintain normal body temperature, which is vital to survival.
- Skeletal muscles provide protection by enclosing internal organs that are vital to survival. Smooth muscles form valves to regulate the passage of substances through tracts in the body. They dilate and constrict the pupils of your eyes. They form the arrector pili muscles found attached to hair follicles. Muscles have so many functions.
Skeletal Muscle
Gross Anatomy
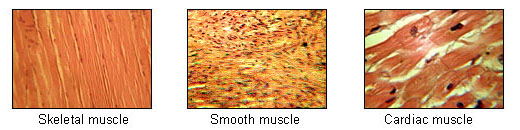
Each of our roughly 650 skeletal muscles is a discrete organ, made of several tissues. The main tissues in skeletal muscles are muscle fibers; however, blood vessels, nerve fibers, and connective tissue are all present in skeletal muscles.
- Each muscle is innervated by a nerve and supplied by blood vessels. The nerve is responsible for stimulating the muscle, producing contractions.
- Blood supply is vital to muscles; they use huge amounts of energy, requiring constant delivery of oxygen and nutrients via arteries; they produce many metabolic wastes that are removed via veins; tiny capillaries actually help accommodate for changes in muscle length during contraction.
- Connective tissue sheaths help support cells and hold the muscle together as a whole.
- On the outside, the epimysium is composed of dense irregular connective tissue that surrounds the muscle.
- Inside of each muscle is an abundance of fascicles, which are basically bundles of sticks (except the sticks are muscle fibers). Each fascicle is surrounded by a layer of fibrous connective tissue, the perimysium.
- Inside of each fascicle is an abundance of individual muscle fibers, each of which is surrounded by a sheath of fine areolar connective tissue, the endomysium.
Skeletal muscles work together with bones, ligaments, tendons, and other connective tissues to produce movement (it’s in the name, after all). Most skeletal muscles attach to bones in at least two places, an insertion and an origin. During muscle contraction, the insertion moves towards the origin (the origin stays in place, just like on a coordinate plane). Muscles may be attached directly or indirectly, the latter of which is much more common.
Microscopic Anatomy
Let’s examine a single skeletal muscle fiber. It is essentially just a long, cylindrical cell. Each muscle fiber has multiple oval-shaped nuclei underneath its sarcolemma (the plasma membrane of skeletal muscle fibers). Their diameter is quite large, ranging from ten to a hundred micrometers. Their length is astounding, some up to thirty centimeters long. This is only the case because each muscle fiber is produced by the fusing of hundreds of embryonic cells. Each muscle cell has a sarcoplasm, which is similar to the cytoplasm; the exception is that sarcoplasm has large numbers of glycosomes and myoglobin. It has all the organelles that you would expect to find in any given cell. In addition to this, it has myofibrils, a sarcoplasmic reticulum, and T-tubules. These structures are vital to muscle contraction.
- Hundreds to thousands of myofibrils can be found in a single muscle fiber. These myofibrils, which run in the same direction as muscle fibers, are very tightly packed; they take up 80% of the cell’s volume. Myofibrils contain sarcomeres, which are responsible for contraction. These sarcomeres contain three types of myofilaments.
- The thick filaments, which are found primarily in the center, contain myosin.
- The thin filaments, which are found primarily towards the sides, contain actin. These also contain tropomyosin, which blocks myosin-binding sites on actin, and troponin, which binds to actin, tropomyosin, and calcium ions.
- The elastic filaments, which are composed of titin. Titin is a giant protein that holds the thick filaments in place.
- Myosin, actin, tropomyosin, troponin, and titin all play a role in the cross-bridge cycle, in which proteins slide past each other to generate movement. You may also find proteins such as dystrophin, nebulin, myomesin, and C proteins that also play roles in this cycle.
- The sarcoplasmic reticulum is a smooth endoplasmic reticulum whose tubules surround myofibrils. Most SR tubules run along the long axis of the myofibril; others, called terminal cisterns, run perpendicularly and occur in pairs. The function of the sarcoplasmic reticulum is to regulate the levels of calcium ions within cells. It stores calcium ions, or Ca2+, and releases them when the muscle fiber is stimulated; this gives the final go signal for contraction.
- T-tubules are elongated tubes that run between paired terminal cisterns, forming triads—groups composed of a pair of terminal cisterns as well as a T-tubule. T-tubules are essentially just continuations of the sarcolemma. This means that when electrical impulses travel along the sarcolemma, T-tubules conduct the impulses to every single sarcomere, releasing calcium ions.
The sliding filament model of contraction describes the process in which myosin heads latch onto myosin-binding sites on actin, forming cross-bridges. These cross bridges form and break several times during a single muscle contraction, generating tension at sliding thin filaments toward the center of the sarcomere. As this occurs in sarcomeres throughout a cell, it shortens. When thin filaments slide towards the center of the sarcomere, Z discs are pulled toward the M line. Overall, the I bands shorten, Z discs become closer together, H zones disappear, and A bands move closer together.
Physiology
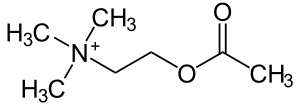
Skeletal muscle fibers are activated by somatic motor neurons, whose axons extend to muscle cells. Each axon ending forms several short, curling branches that form a neuromuscular junction with a single muscle fiber. The axon terminal is very close to the muscle fiber, but they are separated by the synaptic cleft; this space is filled with a gel-like substance. Small membranous sacs, called synaptic vesicles, are located within the axon terminal. These sacs contain acetylcholine, a neurotransmitter (pictured to the right). Where the sarcolemma folds to form the neuromuscular joint, junctional folds provide a surface area for acetylcholine receptors.
- When an action potential reaches an axon terminal, the axon terminal releases acetylcholine into the synaptic cleft. The acetylcholine diffuses across the cleft, attaching to acetylcholine receptors on the sarcolemma. The effects of acetylcholine are quickly terminated by acetylcholinesterase, an enzyme that breaks down acetylcholine to acetic acid and choline; this prevents muscle fibers from contracting without stimulation. The binding of acetylcholine to acetylcholine receptors opens ligand-gated ion channels, increasing the number of sodium ions diffusing in and decreasing the number of potassium ions diffusing out. This causes a change in membrane potential called depolarization.
- The endplate potential (localized depolarization) spreads to adjacent membranes and opens voltage-gated sodium channels, allowing sodium ions to enter. Once the threshold potential is reached, an actional potential is generated. The action potential moves along the sarcolemma, its depolarization wave opening voltage-gated sodium channels in more areas and allowing sodium ions to enter.
- The repolarization wave causes voltage-gated sodium channels to close and voltage-gated potassium channels to open, causing another change in membrane potential called repolarization. During repolarization, muscle fibers are in a refractory period; they are incapable of being stimulated again until repolarization is complete.
Skeletal muscle fibers can be classified as slow fibers and fast fibers on the basis of the velocity at which they shorten. They can also be classified as oxidative fibers or glycolytic fibers on the basis of the pathways they use for forming ATP.
- Slow oxidative fibers contract slowly because their myosin ATPases are slow. They are dependent on oxygen delivery and aerobic pathways. They have high levels of myoglobin (making them red), low stores of glycogen, small fiber diameters, many mitochondria, and many capillaries. All of these qualities make SO fibers best suited for endurance activities.
- Fast oxidative fibers contract quickly because their myosin ATPases are fast. They are dependent on aerobic pathways, though they also use glycolytic reserves. They have high levels of myoglobin (making them red to pink), moderate stores of glycogen, moderate fiber diameters, many mitochondria, and many capillaries. This makes FO fibers best suited for activities such as sprinting and walking.
- Fast glycolytic fibers contract rapidly because their myosin ATPases are fast. They are independent of oxygen and use glycolytic reserves for fuel. They have low levels of myoglobin (making them white), low stores of glycogen, large fiber diameters, few mitochondria, and few capillaries. All of these qualities make FG fibers best suited for short, rapid, intense movements.
The force exerted by a muscle on an object is called muscle tension. The force exerted on the muscle by the weight of the object is called the load.
- If force is exerted by the muscle but the load does not move, muscle fibers do not change lengths; hence, the contraction is an isometric contraction.
- If the force overcomes the load, muscle fibers change lengths; hence, the contraction is an isotonic contraction.
- Concentric contractions are isotonic contractions in which the force overcomes the load and the muscle fiber shortens.
- Eccentric contractions are isotonic contractions in which the force overcomes the load and the muscle fiber lengthens.
All muscles, even while relaxed, are almost always slightly contracted. This phenomenon is called muscle tone. Muscle tone does not produce active movements but instead keeps the muscles firm, healthy, and ready to respond to stimuli. It also assists in joint stabilization and posture maintenance.
Metabolism
Muscle contraction requires energy, which is supplied by ATP. Muscles can only store four to six seconds’ worth of ATP. This means that, since ATP is the only energy source directly used for muscle contraction, ATP must be regenerated as quickly as it is broken down. After ATP is hydrolyzed to ADP and inorganic phosphate, there are three pathways that may regenerate it.
- Direct phosphorylation occurs when creatine phosphate, a high-energy molecule stored in muscles, is used to regenerate ATP. When CP couples with ADP, a phosphate group—plus energy—is transferred from CP to ADP to form ATP almost instantly. This reaction is catalyzed by the enzyme creatine kinase. Muscle cells store about two to three times more CP than ATP, together accounting for about 15 seconds of power for rigorous activity. CP is replenished during rest or inactivity.
- Anaerobic glycolysis is used when stored ATP and CP are exhausted. In this process, ATP is generated by catabolizing glucose from the blood or glycogen from the muscle. This process does not require oxygen, though it can still occur in the presence of oxygen. During glycolysis, glucose is broken down into two pyruvic acid molecules. During less rigorous activities, this pyruvic acid undergoes aerobic respiration; however, it is converted into lactic acid during rigorous activity. This harvests five percent as much ATP from each glucose molecule as aerobic respiration but produces it two and a half times faster. This makes it most useful for thirty to forty seconds of strenuous activity.
- Aerobic respiration produces ninety-five percent of the ATP used during rest, light exercise, and moderate exercise. This process requires oxygen which, when combined with glucose, produces carbon dioxide, water, and ATP. Glycogen is the main source of energy at first, which becomes pyruvic acid, and then fatty acids. It produces a large quantity of ATP but is very slow.
Smooth Muscle
Microscopic Anatomy
Smooth muscle occupies the walls of almost all of the body’s hollow organs, the exception being the heart and other organs. Its muscle fibers are spindle-shaped cells with varying sizes, each with a centralized nucleus. They are only a tenth the width of skeletal muscle fibers and are thousands of times shorter. Smooth muscles lack coarse connective tissue sheaths; instead, they have fine connective tissue—endomysium—between its cells. Typically, smooth muscles are organized into two sheets.
- The longitudinal layer, the outer layer, contains muscle fibers that run parallel to the long axis of the organ. When these muscle fibers contract, it causes the organ to dilate or shorten.
- The circular layer, the inner layer, contains muscle fibers that run around the circumference of the organ. When these muscle fibers contract, it causes the organ to constrict or elongate.
These two layers are continuously contracting and relaxing involuntarily, propelling substances and mixing them together throughout pathways in organs. This action is called peristalsis. This occurs in areas such as the rectum, bladder, and uterus to help the organs expel their contents.
Smooth muscles are innervated by nerve fibers that belong to the autonomic (involuntary) nervous system. Instead of forming neuromuscular junctions, these nerve fibers have bulbous swellings—called varicosities—that form diffuse junctions. In these areas, the varicosities release neurotransmitters into the synaptic cleft.
Smooth muscles have sarcoplasmic reticulum, though they are much less developed than that of skeletal muscles. T-tubules are absent in these; instead, the sarcolemma has multiple caveolae—pouchlike infoldings that sequester bits of extracellular fluid containing calcium ions. Rather than the sarcoplasmic reticulum being responsible for releasing calcium for contraction, extracellular calcium ions are mostly responsible for excitation-contraction coupling.
Smooth muscles, as their name indicates, are not striated. This means that they do not contain sarcomeres. They have myosin and actin filaments, though the ratio of them in smooth muscles is one to thirteen as compared with one to two in skeletal muscles. Smooth muscles compensate for this lack in numbers with their surplus of myosin heads that are situated along the entire length of the muscle, making them just as strong as skeletal muscles. They also lack troponin complexes in actin filaments; rather, a protein called calmodulin is the calcium-binding site. When smooth muscles contract, they twist like corkscrews; this is because their myosin and actin filaments are arranged diagonally.
Physiology
When smooth muscles contract, the whole sheet contracts slowly and synchronously. This is because gap junctions, special connections between cells, allow for action potentials to be transmitted from each muscle fiber to the next. Pacemaker cells in some smooth muscle fibers set the pace of contraction for the entire muscle sheet. The sliding filament model still applies to smooth muscle contraction, as does the utilization of ATP. Smooth muscle contractions are also triggered by rises in intracellular levels of calcium ions.
Calcium activates myosin in smooth muscles by interacting with calmodulin, a calcium-binding protein. Calmodulin interacts with an enzyme called myosin kinase or myosin light chain kinase, which phosphorylates the myosin; this activates the myosin.
In the process of smooth muscle contraction, calcium ions first enter the cytosol from extracellular fluid via voltage-dependent channels or through the SR. Next, the calcium ions bind to calmodulin, activating it. This allows for calmodulin to activate myosin light chain kinase enzymes. These enzymes transfer phosphate to myosin, activating myosin ATPases. The now activated myosin forms cross bridges with actin, shortening smooth muscle fibers.
Smooth muscles contract about thirty times slower than skeletal muscles, but they can maintain the same contractile tension for longer periods of time using less than a percent of the energy cost. In this way, skeletal muscles are like super fast sports cars that run out of gas quickly while smooth muscles are like slower trucks that run out of gas slowly. Just like skeletal muscles, smooth muscles have muscle tone; they maintain a moderate degree of contraction without fatiguing. Smooth muscles only need to produce ATP via aerobic pathways due to their low energy consumption.
Smooth muscle contraction is regulated by neural stimuli, hormones, and localized chemical changes.
- Neural stimuli activate smooth muscles in the same way that they activate skeletal muscles. Neurotransmitter binding generates an action potential, resulting in an increase in calcium ion levels in cytosol. However, some smooth muscles only respond to localized signals. Nerve endings in smooth muscles don’t only release acetylcholine; instead, they release a variety of neurotransmitters that may stimulate different smooth muscle fibers. The way that the body determines which smooth muscle fibers are stimulated is through the type of receptor molecules on the cell’s sarcolemma. Acetylcholine binds to acetylcholine receptors, norepinephrine binds to norepinephrine receptors, etc.
- Some smooth muscles are not innervated by nerves at all. These muscles contract through spontaneous depolarization or in response to chemical stimuli that bind to G protein-linked receptors. Certain hormones, histamine, excess carbon dioxide, low pH, and lack of oxygen all may cause smooth muscles to contract or relax.
Besides smooth muscle tone, slow prolonged contractions, and low energy requirements, smooth muscles have a variety of special features.
- When skeletal muscles are stretched, they respond by contracting vigorously. When smooth muscles are stretched, they also respond by contracting. However, smooth muscles adapt to stretching very quickly, allowing them to relax while still being able to contract when needed. In other words, smooth muscles allow hollow organs to contract and relax slowly without expelling all of their contents. If this weren’t the case, very strange things would occur; your stomach and intestines would expel undigested food and you would not absorb many nutrients from it; your bladder would not be able to hold any urine.
- Smooth muscle stretching generates more tension than skeletal muscle stretching. The way that smooth muscle filaments overlack, in addition to their lack of sarcomeres, allows for them to generate more force. Skeletal muscles can only undergo shortening or lengthening of 30% its length while still functioning efficiently, while smooth muscles can shorten to half their length and lengthen to twice their length.
- All muscle fibers can hypertrophy, causing them to increase in size. Some smooth muscle fibers also undergo hyperplasia, causing them to divide; this increases the number of smooth muscle fibers rather than just their size. A great example is the growing of the uterus in girls during puberty and pregnancy.
Smooth muscles have two major categories: unitary smooth muscle and multi-unit smooth muscle.
- Unitary smooth muscle is found in the walls of all hollow organs except the heart. This is what gives it the nickname visceral muscle. All of the characteristics listed above apply to unitary smooth muscle.
- Multi-unit smooth muscle is found in various forms, such as the arrector pili muscles attached to hair follicles and the internal eye muscles. In these muscles, gap junctions and spontaneous depolarization are possible but rare. These are more similar to skeletal muscles in that their muscle fibers are structurally independent of one another and they have neuromuscular junctions. However, multi-unit smooth muscles are still served by the autonomic (involuntary) nervous system and they can respond to hormones.
Cardiac Muscle
Cardiac muscles can only be found in the walls of the heart. They appear to be striated, just like skeletal muscles. Cardiac muscle is involuntary, as you have no conscious control over the beating of your own heart. Seeing as your entire heart (hopefully) beats at the same time, you could probably guess that cardiac muscle has pacemaker cells that set the tempo for the entire muscle sheet to contract. ATP is produced in cardiac muscles via aerobic pathways, the oxygen being provided by blood vessels in the pulmonary circuit.
Cardiac muscle cells are branched, giving the appearance of chains. Cardiac muscle cells typically have a single nucleus, though they may have two during late fetal development and around birth.
Similar to smooth muscles, cardiac muscles have an endomysium which is attached to the fibrous skeleton of the heart. Their sarcoplasmic reticulums are very similar to those of smooth muscles. Calcium ions for contraction are taken from both the sarcoplasmic reticulum and extracellular fluid, just like in smooth muscles.
Cardiac muscle contraction is slower than skeletal muscles but faster than smooth muscles. Cardiac muscles are unique in that they have myofibrils, like skeletal muscles, but they are of irregular thickness. Gap junctions are present at intercalated discs and neuromuscular junctions are absent. Troponin complexes are present, similar to skeletal muscle. They contain one large T-tubule, rather than two smaller T-tubules, in each sarcomere.
Muscle Development
Most, if not all, of muscle tissues develop from embryonic mesoderm cells called myoblasts.
- In order to form skeletal muscle tissues, several myoblasts must fuse together to form multinucleated myotubes. This process is guided by integrins, a class of cell adhesion proteins. Skeletal muscle tissues start contracting by week seven of embryonic development. Nerve endings release the growth factor agrin as they begin to invade skeletal muscle tissues, activating the enzyme muscle kinase. Satellite cells are myoblast-like cells that help repair injured skeletal muscle fibers, allowing for limited regeneration of dead skeletal muscles.
- In order to form cardiac and smooth muscle tissues, myoblasts develop gap junctions instead of fusing. Cardiac muscle is pumping blood only three weeks after fertilization. It was previously thought that cardiac muscles were incapable of regenerating, though studies have shown that cardiac muscle cells divide modestly. Still, injured cardiac muscle is almost always replaced by scar tissue. Smooth muscles fibers, on the other hand, divide regularly and allow for smooth muscle to regenerate relatively well.
Approximately thirty-six percent of an average woman’s body mass is made up of skeletal muscles, whereas forty-two percent of an average man’s body mass is made up of skeletal muscles. This is primarily due to the effect of testosterone on skeletal muscles rather than the effects of exercise. Due to their amazing resistance to infection, skeletal muscles are rarely affected by homeostatic imbalances, the main exception being a genetic disorder called muscular dystrophy. On a side note, some athletes take doses of steroids, which are essentially synthetic male sex hormones, to increase muscle mass; not only is this illegal, but it is very physiologically dangerous.
Homeostatic Imbalances
| Disease | Description | Cause | Symptoms | Prevention | Treatment |
|---|---|---|---|---|---|
| Poliomyelitis | Poliomyelitis is a viral disease that affects the nerves and can lead to paralysis. There are four types of polio: paralytic, bulbar, spinal, and bulbospinal polio. Paralytic polio destroys motor neurons within the spinal cord and brainstem, inflaming the central nervous system. Spinal polio is the most common form of poliomyelitis. It is a viral invasion of motor neurons; the virus destroys ganglia. Paralysis is rarely seen in fingers and toes, but most often where limbs meet the body. Bulbar polio destroys nerves within the bulbar region of the brain stem. Symptoms include difficulty breathing and swallowing. Bulbospinal polio is a combination of the symptoms of bulbar polio and spinal polio. | Poliomyelitis is caused by infection with the poliovirus. Polio is transmitted through contaminated water and food or contact with an infected person. | Many people who are infected with the poliovirus don't become sick and have no symptoms. However, those who do get sick develop paralysis, which can sometimes be fatal. Other symptoms may include difficulty breathing and swallowing, fever, sore throat, vomiting, no appetite, and stiffness. | There are two ways to prevent polio: passive immunization and vaccines. Passive Immunization involves injecting purified gamma globulin from a polio patient into someone who has contracted polio or a healthy individual. In the former, this may halt polio; in the latter, this may prevent up to 80% of cases. Since it is impractical to obtain enough samples for many people, it is not effective for widespread use. This is where vaccines come in. The inactivated polio vaccine, or the Salk vaccine, ingests a dead strain of each type of poliovirus into one’s body. This produces antibodies in the blood to all three types, preventing the spread of the virus upon infection and protecting against paralysis. This vaccine is expensive and is not very effective in providing the intestine with immunity. The oral polio vaccine is used more often. It may consist of one, two, or all three strains of attenuated polioviruses. Since these are still live, albeit weakened, it is possible for the virus to mutate into the wild-type form. Since the attenuated viruses are excreted from the intestine, other people may be provided passive immunity upon infection if the virus is still attenuated; however, they may contract wild-type poliomyelitis if the virus has mutated. | Treatment includes bed rest, pain relievers, and portable ventilators. |
| Muscular Dystrophies | Muscular dystrophies are a group of inherited diseases that are characterized by weakness and deterioration of muscle tissue. The tissue is slowly replaced by fat, rendering the patient immobile. There are many types of muscular dystrophy, the most common in children being Duchenne muscular dystrophy. This form only affects males; most with DMD die in their late teens or early twenties. Myotonic muscular dystrophy is the most common type in adults. Most with MMD have decreased life expectancies. There are several more forms of muscular dystrophy, the most prevalent being the two listed above as well as Becker and facioscapulohumeral muscular dystrophy. | The DMD gene, the largest known gene in humans, provides instructions for producing a protein called dystrophin. Dystrophin is responsible for strengthening muscle fibers and protecting them from injury. Each different mutation of this gene causes a different form of muscular dystrophy, most of these mutations being inherited. | Symptoms include progressively weakness in damaged muscles, leading to the need for a wheelchair. Other symptoms include trouble breathing or swallowing. | As muscular dystrophies are genetic diseases, there are currently no ways to prevent them. | There are no cures for muscular dystrophies, but corrective surgery, exercise, and physical therapy can help patients’ condition improve. |
| Myasthenia Gravis | Myasthenia gravis is a chronic autoimmune disease that causes weakness and rapid fatigue of voluntary muscles. | Myasthenia gravis is caused by the blocking of acetylcholine receptors by antibodies in the neuromuscular junction, hindering the communication between the nervous and muscular systems. | Symptoms of myasthenia gravis include weakness in the arms and legs, eyelids drooping, difficulty chewing and swallowing, double vision, and difficulty talking. | Since myasthenia gravis is caused by an error in the transmission of nerve impulses to muscles, it is not currently preventable. | Myasthenia gravis can be treated with medications such as anticholinesterase agents and immunosuppressive drugs, as well as surgeries such as thyroidectomies. |
| Tetanus | Tetanus is an extremely rare and serious bacterial infection that causes painful muscle spasms and often leads to death. | Tetanus is caused by bacterial infection by the bacterium Clostridium tetani, which produces a neurotoxin called tetanospasmin. | Tetanus causes painful muscle spasms primarily in the jaw and neck, as well as the chest, back, and abdominal muscles; this often leads to fractures and muscle tears. Tetanus may also cause difficulty breathing, fever, irritability, and difficulty swallowing. | Tetanus cannot be prevented in any way except for the Tdap vaccine, which contains the tetanus toxoid. This vaccine is effective against tetanus, diphtheria, and pertussis. | Treatment for tetanus is focused on managing symptoms. Antibiotics, bedrest, tetanus immunoglobulin, muscle relaxers, sedatives, and surgery all may help with this. |
| Myositis | Myositis is a term that refers to inflammation of muscles. | Myositis can be caused by many diseases; it is typically caused by infections, injuries, autoimmune diseases, and drugs. | Myositis is often accompanied by muscle weakness and muscle pain, tiredness and fatigue, trouble climbing stairs, standing from a seated position, or reaching up, and difficulty swallowing. | Myositis is caused by many diseases, of which only infectious and drug-induced myositis are preventable. Infectious myositis can be prevented by getting flu shots and vaccinations and thoroughly cooking meats. Drug-induced myositis can be prevented by avoiding unprescribed drugs, injecting drugs into a clean site if prescribed, and adhering to the instructions given on the prescription. | Myositis cannot be cured, but it can be treated using corticosteroids, immunosuppressants, anti-inflammatory drugs, exercise, rest, nutrition, and reduction of stress. |
| Carpal Tunnel Syndrome | Carpal tunnel syndrome is a numbness and tingling in the hand and arm caused by a pinched nerve in the wrist. | Carpal tunnel syndrome is caused by a pinched nerve in the wrist, namely the median nerve. This may be caused by repetitive motions of the hand or wrist. | Carpal tunnel syndrome causes numbness and tingling in the thumb-side of the hand or the palm of the hand. Pain may extend to the elbow, wrist, or hand. This causes problems with coordination in the hand, as well as weakness in the hand. | Carpal tunnel syndrome can be prevented by avoiding repetitive motions or through the usage of ergonomic aids. | Carpal tunnel syndrome can be treated by using a splint, applying heat or ice, reducing stress on the wrist, anti-inflammatory drugs, and carpal tunnel release surgery. |
| Botulism | Botulism is an extremely rare and potentially fatal poisoning caused by a bacterial infection. | Botulism is caused by toxins produced by Clostridium botulinum, a bacterium that may infect the body. | The main symptoms of botulism include difficulty swallowing or speaking, facial weakness, and paralysis. | Botulism can be prevented by properly refrigerating foods if they are not being eaten, cooking food thoroughly, and avoiding eating food from damaged or bulging containers. | Botulism can be treated by an antitoxin injection and breathing assistance. |
| Fibromyalgia | Fibromyalgia, or fibrositis, is a disease causing widespread musculoskeletal pain, fatigue, and issues with sleep, memory, and mood. | The cause of fibromyalgia is unknown, but it is linked to traumatic injuries, rheumatoid arthritis, and other autoimmune disorders. | Fibromyalgia causes long-term, mild-to-severe, body-wide pain and tender points in joints, muscles, tendons, and other soft tissues. | There is no known way to prevent fibromyalgia; however, remaining healthy by maintaining a good diet, safely exercising, and resting well may help prevent any medical condition, including fibromyalgia. | Fibromyalgia can be treated using SSRIs (selective serotonin reuptake inhibitors), analgesics, NSAIDs (non-steroidal anti-inflammatory drugs), nerve pain medications, and muscle relaxants. Physical therapy and counseling may also help treat fibromyalgia. In mild cases, symptoms may go away when stress is decreased or lifestyle changes are implemented |
| Chronic Fatigue Syndrome | Chronic fatigue syndrome, or myalgic encephalomyelitis, is a chronic disease—occurring more often in women than men—characterized by fatigue worsened by activity and unimproved by rest. | The cause of chronic fatigue syndrome is unknown, though it mainly affects women from ages thirty to fifty. | Chronic fatigue syndrome is associated with extreme fatigue lasting at least six months; it worsens with activity but does not improve with rest. This severely inhibits your ability to do many activities. | There are no known ways to prevent chronic fatigue syndrome. | Chronic fatigue syndrome cannot be cured, but it can be treated by maintaining a healthy diet, using antidepressants, undergoing cognitive behavioral therapy, and undergoing graded exercise and relaxation techniques. |
Musculoskeletal Interactions
As a muscle shortens, its insertion—its attachment to the movable bone—moves towards its origin—its fixed point of attachment. Every action that a muscle or group of muscles is able to perform is an action that another muscle or another group of muscles can “undo.”
There are four functional groups of skeletal muscles: prime movers, antagonists, synergists, and fixators.
- A prime mover, or agonist, is a muscle that has a major responsibility for producing a specific movement. For example, the pectoralis major is a prime major of arm flexion.
- Muscles that “undo” the movements of agonists are called antagonists. In this way, agonists and antagonists work together in antagonistic pairs. Just because a muscle is a prime mover does not mean that it cannot be an antagonist. For example, the latissimus dorsi is the antagonist for undoing flexion of the arm. All the while, it is also the prime mover for extension of the arm.
- Many movements, in addition to the two aforementioned groups, involve the action of one or more synergists. These muscles assist prime movers by adding extra force or by reducing unnecessary movements. For example, you are able to make a fist shape without bending your wrist because of synergists; they stabilize the wrist. As another example, flexors may produce undesirable movements that synergists prevent.
- Synergists that immobilize a muscle’s origin—in other words, immobilize a bone—in order to provide a stable base for a prime mover are called fixators. For example, the scapula is freely movable, being attached to the axial skeleton only by muscles. In order to immobilize the scapula during shoulder movements, fixator muscles act. Any muscles that help maintain upright posture are also fixators.
In order to understand what each muscle does, they are named according to their location, shape, size, direction of muscle fibers, number of origins, location of attachments, and/or actions. Some muscles, like the extensor carpi radialis longus (its action is extension, it acts on the carpus—or wrist—it is located near the radius, and is long compared to other wrist extensors), may be highly descriptive. Other muscles, like the gastrocnemius (gaster means stomach and kneme means leg), are not very descriptive.
The arrangement of fascicles in muscles contributes to how much force they produce and the speed at which they do it. Recall that fascicles are just bundles of muscle fibers.
- Fascicles may be arranged in a circular pattern when they look like concentric rings. Muscles with circular fascicle arrangements are sphincters, which close external body openings by contracting. For example, the orbicularis muscles around the eyes and mouth close the eyes and mouth when they contract.
- Fascicles may also be arranged in a convergent pattern when they have a broad origin and converge towards a single tendon of insertion. These muscles look like triangles or fans, like the pectoralis major.
- Fascicles may be arranged in a parallel pattern when they run parallel to the long axis of the muscle. This occurs in straplike muscles such as the sartorius, as well as in spindle-shaped muscles such as the biceps brachii. However, the latter may be classified separately as fusiform muscles.
- Fascicles may be arranged in a pennate pattern when they are short and attach obliquely to a central tendon that runs the length of the muscle.
- Unipennate muscles are muscles in which the fascicles insert into only one side of the tendon, such as the extensor digitorum longus.
- Bipennate muscles are muscles in which the fascicles insert into the tendon from opposite sides, such as the rectus femoris. This looks similar to a feather.
- Multipennate muscles are muscles in which the fascicles insert into the tendon from many sides, such as the deltoid muscle. This looks like multiple feathers.
An important topic to understand is lever systems. These can describe everyday objects like seesaws and shovels, but they can also describe the relationships between bones and muscles. A lever is basically just a rigid bar that moves on a fixed point, the fulcrum, when force is applied to it. The applied force, called effort, is used to move a resistance, or load. In the human body, the joints are the fulcrums while the bones are the levers; muscle contractions provide the efforts, while the bones and any overlying tissues are the loads. A power lever operates with a mechanical advantage; the load is close to the fulcrum and the effort is applied far from the fulcrum. A speed lever operates with a mechanical disadvantage; the load is far from the fulcrum and the effort is applied near the fulcrum.
- In a first-class lever, the effort is applied at one end of the lever and the load is at the other; the fulcrum is situated between the effort and the load. Think of a seesaw; when you apply downward force to one side of the seesaw, the other side moves about the center of the seesaw. These can be both strength and speed levers.
- In a second-class lever, the effort is applied at one end of the lever and the fulcrum is at the other; the load is situated between the effort and the fulcrum. Think of a wheelbarrow; when you push the handle, the wheel moves forward and carries the tray. These are strength levers; they are uncommon in the body.
- In a third-class lever, the effort is applied between the load and the fulcrum. Think of barbecue tongs; you apply inward force to the middle of the handle in order to grasp the meat. Meanwhile, the fulcrum is where the sides of the tongs connect. These are speed levers; they are the most common class of levers in the body.
Major Skeletal Muscles
| Muscle | Description | Origin | Insertion | Action | Nerve |
|---|---|---|---|---|---|
| Frontalis | The frontalis is the frontal belly of the occipitofrontalis. It covers the forehead and the dome of the skull. | Its origin is the epicranial aponeurosis. | Its insertion is the skin of the eyebrows and the root of the nose. | When the epicranial aponeurosis is fixed, the frontalis raises the eyebrows. It wrinkles the forehead skin horizontally. | It is supplied by cranial nerve VII, the facial nerve. |
| Occipitalis | The occipitalis is the occipital belly of the occipitofrontalis. It covers the lateral two-thirds of the superior nuchal line. | Its origin points are the occipital and temporal bones. | Its insertion is the epicranial aponeurosis. | The occipitalis fixes the aponeurosis and pulls the scalp posteriorly. | It is supplied by cranial nerve VII, the facial nerve. |
| Orbicularis oris | The orbicularis oris is a multilayered muscle of the lips. | It arises indirectly from the maxilla and mandible. | It inserts into the tissues of the upper and lower lips. | The orbicularis oris closes the lips, purses and protrudes the lips, and produces kissing and whistling motions. | It is supplied by cranial nerve VII, the facial nerve. |
| Orbicularis oculi | The orbicularis oris is a thin, flat sphincter that surrounds the rim of the orbit. | Its origin points are the frontal and maxillary bones and the ligaments surrounding the orbit. | It inserts into the tissue of the eyelid. | The orbicularis oris closes the eyes, produces blinking and squinting, and draws the eyebrows inferiorly. | It is supplied by cranial nerve VII, the facial nerve. |
| Orbicularis oculi | The orbicularis oris is a thin, flat sphincter that surrounds the rim of the orbit. | Its origin points are the frontal and maxillary bones and the ligaments surrounding the orbit. | It inserts into the tissue of the eyelid. | The orbicularis oris closes the eyes, produces blinking and squinting, and draws the eyebrows inferiorly. | It is supplied by cranial nerve VII, the facial nerve. |
| Zygomaticus major | The zygomaticus major is a paired muscle that extends diagonally from the cheekbone to the corner of the mouth. | It originates from the zygomatic bone. | It inserts into the skin and muscles at the corner of the mouth. | It raises the lateral corners of the mouth upwards; in other words, it produces smiling. | It is supplied by cranial nerve VII, the facial nerve. |
| Masseter | The masseter is a paired, powerful muscle that covers the lateral aspect of the mandibular ramus. | It originates from the zygomatic bone and the rest of the zygomatic arch. | It inserts into the mandibular angle and the mandibular ramus. | It closes the jaw, elevates and retracts the mandible, and maintains the resting position of the mandible. | It is supplied by cranial nerve V, the trigeminal nerve. |
| Sternocleidomastoid | The sternocleidomastoid is a paired, two-headed muscle on the anterolateral surface of the neck. | It originates from the manubrium of the sternum and the medial portion of the clavicle. | It inserts into the mastoid process of the temporal bone and the superior nuchal line of the occipital bone. | It flexes and laterally rotates the head. | It is supplied by cranial nerve XI, the accessory nerve, as well as the ventral rami of C2 and C3. |
| Trapezius | The trapezius is a paired, superficial muscle of the posterior thorax; it is triangular. | It originates from the occipital bone, the ligamentum nuchae, and the spinous processes of C7 through T12. | It inserts continuously along the acromion and the spine of the scapula and the lateral third of the clavicle. | It stabilizes, raises, retracts, and rotates the scapula. | It is supplied by cranial nerve XI, the accessory nerve, as well as C3 and C4. |
| Buccinator | The buccinator is a paired, thin, horizontal musse; it is the principal muscle of the cheek. | It originates from the alveolar process of the maxilla and mandible. | It inserts into the orbicularis oris. | It compresses the cheek, holds food between teeth during chewing, and draws the corner of the mouth laterally. | It is supplied by cranial nerve VII, the facial nerve. |
| External Intercostals | The eleven pairs of external intercostals lie between the ribs. | They originate from the inferior borders of the ribs above them. | They insert into the superior borders of the ribs below them. | They pull the ribs towards one another to elevate the rib cage. They aid in inspiration and are synergists of the diaphragm. | They are supplied by the intercostal nerves. |
| Internal Intercostals | The eleven pairs of internal intercostals lie between the ribs. | They originate from the superior borders of the ribs below them. | They insert into the inferior borders of the ribs above them. | They draw the ribs together and depress the rib cage. | They are supplied by the intercostal nerves. |
| Transverse abdominis | The transverse abdominis is the innermost paired muscle of the abdominal wall. | It originates from the inguinal ligament, the lumbar fascia, the cartilages of the last six pairs of ribs, and the iliac crest. | It inserts into the linea alba, the pubic crest, the last three or four pairs of ribs, and the costal margin. | As a pair, it flexes the vertebral column and compresses the abdominal wall; as individuals, they rotate the trunk and flex laterally. | They are supplied by the intercostal nerves of T7 through L1. |
| Infraspinatus | The infraspinatus is a paired, thick, triangular muscle of the scapula. | It originates from the infraspinous fossa of the scapula. | It inserts into the superior part of the greater tubercle of the humerus. | It initiates abduction of the arm, stabilizes the shoulder joint, and prevents the humerus from being dislocated. | It is supplied by the suprascapular nerve. |
| Rectus abdominis | The rectus abdominis muscles are a medial superficial pair of muscles that extend from the pubis to the ribcage. | It originates from the pubic crest and pubic symphysis. | It inserts into the xiphoid process and the costal cartilages of rib pairs five through seven. | It flexes and rotates the lumbar region of the vertebral column, fixes and depresses the ribs, and stabilizes the pelvis during walking. | It is supplied by the intercostal nerves of T6 through T12. |
| Serratus anterior | The serratus anterior is a paired, fan-shaped muscle that forms the medial wall of the axilla. | It originates from a series of muscle slips from rib pairs one through nine. | It inserts into the anterior surface of the vertebral border of the scapula. | It rotates the scapula so that its inferior angle moves laterally and upwards. | It is supplied by the long thoracic nerve. |
| Diaphragm | The diaphragm is a broad muscle that forms the floor of the thorax. | It originates from the inferior, internal surface of the ribcage and sternum, as well as the costal cartilages of the last six ribs and lumbar vertebrae. | It inserts into the central tendon. | It is the prime mover of inspiration; it flattens during contraction, increasing the vertical dimensions of the thorax. | It is supplied by the phrenic nerves. |
| Pectoralis major | The pectoralis major is large, paired, fan-shaped muscle covering the superior portion of the chest. | It originates from the sternal end of the clavicle, the sternum, the cartilage of rib pairs one through seven, and the aponeurosis of the external oblique muscle. | It inserts by a short tendon into the intertubercular sulcus and the greater tubercle of the humerus. | It is the prime mover of arm flexion; it rotates the arm medially and adducts the arm. | It is supplied by the lateral and medial pectoral nerves. |
| Latissimus dorsi | The latissimus dorsi is a broad, flat, paired, triangular muscle of the lower back. | It originates from the lower six thoracic vertebrae, the lumbar vertebrae, the four lowest rib pairs, the iliac crest, and the inferior scapular angle. | It inserts into the floor of the intertubercular sulcus of the humerus. | It is the prime mover of arm extension; it is a powerful arm adductor; it medially rotates the arm at the shoulder. | It is supplied by the thoracodorsal nerve. |
| Deltoid | The deltoid is a thick, paired, triangular, multipennate muscle at the shoulder. | It originates from the lateral part of the clavicle, the acromion, and the spine of the scapula. | It inserts into the deltoid tuberosity of the humerus. | It is the prime mover of arm abduction and the antagonist of the pectoralis major and the latissimus dorsi. | It is supplied by the axillary nerve. |
| Teres major | The teres major is a thick, paired, rounded muscle on the posterior wall of the axilla. | It originates from the lateral border of the dorsal scapular surface. | It inserts into the greater tubercle of the humerus. | It rotates the humerus laterally and stabilizes the shoulder joint. | It is supplied by the axillary nerve. |
| Biceps brachii | The biceps brachii is a paired, two-headed fusiform muscle. | Its short head originates from the coracoid process, its long head from the supraglenoid tubercle and the lip of the glenoid cavity. | It inserts into the radial tuberosity by the common tendon. | It flexes the elbow joint and supinates the forearm, usually simultaneously. | It is supplied by the musculocutaneous nerve. |
| Triceps brachii | The triceps brachii is a large, paired, fleshy, three-headed muscle on the posterior compartment of the arm. | Its long head originates from the infraglenoid tubercle of the scapula, its lateral head from the posterior shaft of the humerus, and its medial head from the posterior humeral shaft. | It inserts into the olecranon of the ulna by the common tendon. | It is the prime mover of forearm extension and the antagonist of forearm flexion. | It is supplied by the radial nerve. |
| Brachialis | The brachialis is a strong, paired muscle deep to the biceps brachii. | It originates from the front of the distal humerus. | It inserts into the coronoid process of the ulna and the capsule of the elbow joint. | It is a major forearm flexor. | It is supplied by the musculocutaneous nerve. |
| Brachioradialis | The brachioradialis is a paired, superficial muscle of the lateral forearm | It originates from the lateral supracondylar ridge at the distal end of the humerus. | It inserts into the base of the radial styloid process. | It is a synergist in forearm flexion. | It is supplied by the radial nerve. |
| Palmaris longus | The palmaris longus is a small, paired, fleshy muscle that is often absent. | It originates from the medial epicondyle of the humerus. | It inserts into the palmar aponeurosis, the fascia of the palm. | It tenses the skin and fascia of the palm during hand movements; it is a weak wrist flexor and a weak synergist for elbow flexion. | It is supplied by the median nerve. |
| Flexor carpi radialis | The flexor carpi radialis is a paired muscle that runs diagonally across the forearm. | It originates from the medial epicondyle of the humerus. | It inserts into the base of the second and third metacarpals. | It is a powerful flexor of the wrist, abducts the hand, and is a weak synergist of elbow flexion. | It is supplied by the median nerve. |
| Flexor digitorum superficialis | The flexor digitorum superficialis is a paired, two-headed muscle at the distal end of the forearm. | It originates from the medial epicondyle of the humerus, the coronoid process of the ulna, and the shaft of the radius. | It inserts into the middle phalanges of the second through fifth fingers by four separate tendons. | It flexes the wrist and the middle phalanges of the second through fifth fingers. | It supplies the median nerve. |
| Extensor carpi radialis | The extensor carpi radialis is a paired muscle that parallels the brachioradialis on the lateral forearm. | It originates from the lateral supracondylar ridge of the humerus. | It inserts into the base of the second metacarpal. | It helps extend the wrist and abduct the wrist. | It is supplied by the radial nerve. |
| Extensor digitorum | The extensor digitorum is a paired muscle that lies medial to the extensor carpi radialis brevis, which lies deep to the extensor carpi radialis. | It originates from the lateral epicondyle of the humerus. | It inserts into the distal phalanges of the second through fifth fingers by four separate tendons. | It is the prime mover of finger extension; it extends the wrist and abducts the fingers. | It is supplied by the posterior interosseous branch of the radial nerve. |
| Extensor digiti minimi | The extensor digiti minimi is a detached portion of the extensor digitorum. | It originates from the lateral epicondyle of the humerus. | It inserts into the distal phalanges of the second through fifth fingers by four separate tendons. | It extends the fifth finger. | It is supplied by the posterior interosseous branch of the radial nerve. |
| Extensor carpi ulnaris | The extensor carpi ulnaris is a long, paired, slender muscle. | It originates from the lateral epicondyle of the humerus and the posterior border of the ulna. | It inserts into the base of the fifth metacarpal. | It helps extend the wrist and adduct the wrist. | It is supplied by the posterior interosseous branch of the radial nerve. |
| Iliopsoas | A composite of two paired muscles: the iliacus and the psoas major. The iliacus is large, fan-shaped, and more lateral. The psoas major is longer, thicker, and more medial. | The iliacus originates from the iliac fossa, the iliac crest, and the ala of the sacrum. The psoas major originates from the transverse processes, transverse bodies, and the discs of T12 through L5. | The iliacus inserts into the lesser trochanter of the femur via the iliopsoas tendon. The psoas major inserts into the lesser trochanter of the femur via the iliopsoas tendon. | The iliopsoas is the prime mover for thigh flexion; it also is an important postural muscle. | The iliacus is supplied by the femoral nerve. The psoas major is supplied by the ventral rami. |
| Sartorius | The sartorius is a paired, straplike, superior muscle running obliquely across the anterior surface of the thigh to the knee; it is the longest muscle in the body. | It originates from the anterior superior iliac spine. | It inserts into the medial aspect of the proximal tibia. | It flexes, abducts, and laterally rotates the thigh; it is a weak knee flexor. | It is supplied by the femoral nerve. |
| Gluteus maximus | The gluteus maximus is the largest and most superficial paired gluteus muscle. | It originates from the dorsal ilium, sacrum, and coccyx. | It inserts into the gluteal tuberosity of the femur and the iliotibial tract. | It is a major extensor of the thigh. | It is supplied by the inferior gluteal nerve. |
| Gluteus medius | The gluteus medius is a thick, paired muscle covered by the gluteus maximus. | It originates from between the anterior and posterior gluteal lines on the lateral surface of the ilium. | It inserts into the lateral aspect of the greater trochanter of the femur by the short tendon. | It abducts and medially rotates the thigh. | It is supplied by the superior gluteal nerve. |
| Tensor fasciae latae | The tensor fascia latae is enclosed between the fascia layers of the anterolateral aspect of thigh. | It originates from the anterior aspect of the iliac crest and the superior iliac spine. | It inserts into the iliotibial tract. | It steadies the knee and the trunk on the thigh by making the iliotibial tract taut. | It is supplied by the superior gluteal nerve. |
| Adductor longus | The adductor longus is the most anterior paired adductor muscle. | It originates near the pubic symphysis. | It inserts into the linea aspera. | It adducts, flexes, and medially rotates the thigh. | It is supplied by the obturator nerve. |
| Gracilis | The gracilis is a long, thin, paired, superficial muscle of the medial thigh. | It originates from the inferior ramus and the body of the pubis and the adjacent ischial ramus. | It inserts into the medial surface of the tibia just inferior to the medial condyle. | It adducts the thigh and flexes and medially rotates the leg. | It is supplied by the obturator nerve. |
| Semimembranosus | The semimembranosus is a paired muscle deep to the semitendinosus. | It originates from the ischial tuberosity. | It inserts into the medial condyle of the tibia via the oblique popliteal ligament. | It extends the thigh and flexes the knee. | It is supplied by the obturator nerve. |
| Semitendinosus | The semitendinosus is a fleshy, paired muscle that lies medial to the biceps femoris. | It originates from the ischial tuberosity. | It inserts into the medial aspect of the upper tibial shaft. | It extends the thigh and flexes the knee. | It is supplied by the sciatic nerve. |
| Biceps femoris | The biceps femoris is the most lateral of the paired hamstring muscles. | Its long head originates from the ischial tuberosity. Its short head originates from the linea aspera, the lateral supracondylar line, and the distal femur. | It inserts into the head of the fibula and the lateral condyle of the tibia via the common tendon. | It extends the thigh and flexes the knee. | It is supplied by the tibial portion of the sciatic nerve. |
| Rectus femoris | The rectus femoris is a paired, superficial muscle of the anterior thigh; it is one of four heads of the quadriceps femoris. | It originates from the anterior inferior iliac spine and the superior margin of the acetabulum. | It inserts into the patella and tibial tuberosity via the patellar ligament. | It extends the knee and flexes the thigh at the hip. | It is supplied by the femoral nerve. |
| Vastus lateralis | The vastus lateralis is a paired muscle that forms the lateral aspect of the thigh; it is the largest of the four heads of the quadriceps femoris. | It originates from the greater trochanter, the intertrochanteric line, and the linea aspera. | It inserts into the patella and tibial tuberosity via the patellar ligament. | It extends and stabilizes the knee. | It is supplied by the femoral nerve. |
| Vastus intermedius | The vastus intermedius lies between the vastus lateralis and the vastus medialis on the anterior thigh. | It originates from the anterior and lateral surfaces of the proximal shaft of the femur. | It inserts into the patella and tibial tuberosity via the patellar ligament. | It extends the knee. | It is supplied by the femoral nerve. |
| Vastus medialis | The vastus medialis forms the inferomedial aspect of the thigh. | It originates from the linea aspera, intertrochanteric line, medial supracondylar line. | It inserts into the patella and tibial tuberosity via the patellar ligament. | It extends the knee. | It is supplied by the femoral nerve. |
| Tibialis anterior | The tibialis anterior is a paired, superficial muscle of the anterior leg. | It originates from the lateral condyle and the upper two-thirds of the tibial shaft. | It inserts into the inferior surface of the medial cuneiform and the first metatarsal by a tendon. | It is the prime mover of dorsiflexion; it inverts the foot. | It is supplied by the deep fibular nerve. |
| Gastrocnemius | The gastrocnemius is the superficial muscle of the two paired muscles of the triceps surae located in the calf. | It originates from the medial and lateral condyles of the femur. | It inserts into the posterior calcaneus via the calcaneal tendon. | It is a plantar flexor when the knee is extended; it is a knee flexor when the foot is dorsiflexed. | It is supplied by the tibial nerve. |
| Soleus | The soleus is the broad, flat, deep muscle of the two paired muscles of the triceps surae located in the calf. | It originates from the superior tibia, the fibula, and the interosseous membrane. | It inserts into the posterior calcaneus via the calcaneal tendon. | It is a plantar flexor, an important locomotor, and a postural muscle. | It is supplied by the tibial nerve. |
| Peroneus longus | The peroneus longus is a paired, superficial lateral muscle overlying the fibula. | It originates from the head and upper portion of the lateral fibula. | It inserts into the first metatarsal and the medial cuneiform by the long tendon. | It is a plantar flexor and everts the foot. | It is supplied by the superficial fibular nerve. |
| Peroneus brevis | The peroneus brevis is a paired, smaller muscle deep to the peroneus longus. | It originates from the distal fibula shaft. | It inserts into the proximal end of the fifth metatarsal. | It is a plantar flexor and everts the foot. | It is supplied by the superficial fibular nerve. |
Useful Links
- AnatomyAtlases - Muscles of the Face and Neck - 9
- AnatomyAtlases - Muscles of the Palate, Jaw, Neck, and Back - 10
- AnatomyAtlases - Muscles of the Face, Trunk, Arms, and Feet - 11
- AnatomyAtlases - Muscles of the Torso and Arms - 12
- AnatomyAtlases - Muscles of the Abdomen, Pelvis, and Arm - 13
- AnatomyAtlases - Muscles of the Anterior and Lateral Surface of the Legs - 14
- AnatomyAtlases - Muscles of the Dorsal and Medial Surface of the Legs - 15
- East Tennessee State University - Histology of Muscle
- Eastern Kentucky University - Muscle
- GetBodySmart - Muscular System
- Khan Academy - The Musculoskeletal System
- Loyola University Chicago - Master Muscle List
- Marymount High School - Muscles
- San Diego State University - Actin Myosin Crossbridge 3D Animation
- University of California San Diego - Muscle Physiology
- University of Wisconsin-La Crosse - Human Skeletal Muscle Anatomy
- University of Wisconsin-La Crosse - Histology of Muscle Tissue