Anatomy/Integumentary System
The integumentary system or integument is a focus topic of the event Anatomy. It came into rotation for the 2014, 2015, and 2016 seasons. It will once again be a focus for the 2020 season, and rotates concurrently with the skeletal and muscular systems. The integumentary system is composed of skin, hair, nails, and glands.
Functions
In an average adult, the integumentary system has a surface area of 1.5-2.0 square meters and weighs 4 to 5 kilograms. It varies in thickness from 0.5 mm on the covering of the eyelids to 4 mm on the palms and soles. The integumentary system serves many functions, the main of which are listed below.
- Protection: The integumentary system's main function is to protect your body from injury and pathogens. For example, the stratum germinativum repairs minor injuries. Additionally, the skin acts as a barrier to protect from pathogens. Keratin and glycolipids in the skin help waterproof it and the continuity of the skin protects from bacterial invasion. There are also chemical barriers such as skin secretions of sebum, human defensins, and cathelicidins. The acid mantle of the skin causes the skin to have a low pH which slows bacterial growth on the skin's surface. Melanin protects the body from UV damage. Additionally, Langerhans' cells and dermal macrophages are located in the skin and activate the immune system. The structure of DNA in the skin allows its electrons to absorb UV radiation and convert it into heat.
- Temperature maintenance: The integumentary system also regulates heat exchange with the environment and keeps the body at an average of 98.6 °F or 36.0 °C. Sweat, secreted by sudoriferous glands, helps cool the body. Dilation and constriction of blood vessels in the skin also helps to regulate the body temperature.
- Synthesis and storage: The integumentary system synthesizes Vitamin D3 and stores lipids in adipose (fat) tissue.
- Sensory reception: There are touch, pressure, pain, and temperature sensory receptors in the skin which interact with the nervous system. Meissner's corpuscles and Merkel disks sense light touch while Pacinian receptors, located deeper in the dermis, detect deep pressure. Hair follicle receptors sense movement of hairs. Nociceptors and bare nerve endings sense pain. Thermoreceptors sense heat and cold.
- Excretion and secretion: The skin excretes saltwater and organic wastes. In postpubescent females, modified glands called mammary glands secrete milk. Sudoriferous (sweat) glands are identified into two types- apocrine and eccrine. Eccrine sweat glands secrete cooling sweat and apocrine sweat glands secrete during emotional stress or excitement. Ceruminous glands are modified sweat glands that produce ear wax.
- Hydration: The integumentary system protects the body from dehydration.
Structure of the Skin
- 3 Major Layers of the Skin
- The epidermis is the outer, thinner layer that consists of epithelial tissue.
- The dermis is the inner, thicker layer that consists of connective tissue.
- The hypodermis—also known as the subcutaneous or subQ layer—is located underneath the dermis; it is not necessarily part of the integument but shares some functions. It is composed of areolar/adipose connective tissues that anchor skin to the underlying structures—mostly muscles—and insulates/absorbs shock
Epidermis
- The epidermis is composed primarily of keratinized stratified squamous epithelium.
- The epidermis contains four major types of cells.
- Keratinocytes produce keratin, a tough insoluble fibrous protein that provides protection and contributes to the strength and water resistance displayed by the epidermis, hair and nails.
- Melanocytes produce melanin, a pigment that determines skin color.
- Langerhans cells, or dendritic cells, are macrophages that originate in the red bone marrow. They are involved in the immune response.
- Merkel cells function in the sensation of touch along with the other adjacent tactile discs (receptors).
- The epidermis contains four major types of cells.
- Skin can be classified as thin (hairy) or thick (hairless/glabrous skin).
- Thin skin, or hairy skin, covers all body regions except for the palms, fingertips, and soles. It is usually 1-2 millimeters thick. Thin skin has fewer skin receptors and sudoriferous glands and more sebaceous glands than thick skin.
- Thick skin, also known as hairless or glabrous skin, covers the palms, fingertips, and soles. Thick skin has more skin receptors and sudoriferous glands and fewer sebaceous glands. Skin ridges (e.g. fingerprints) are found due to well-developed dermal papillae. Skin ridges aid in grip and object manipulation.
Epidermal Layers
- The epidermis is composed of four layers in thin skin, and five layers in thick skin. The layers are as follows, starting from the deepest to the shallowest.
- The basal layer, stratum basale, or stratum germinativum.
- The stratum basale is the deepest epidermal layer. It is the "growing layer of the skin" or the "base of it" (hence its other name, stratum basale).
- It is connected by hemidesmosomes, which are special disc-shaped proteins, to the basement membrane, which is a network of protein fibers separating the epidermis from the dermis below.
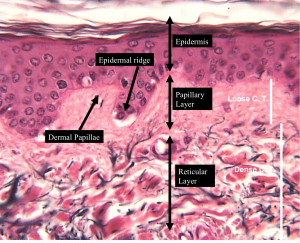
- The stratum basale, as pictured above, descends into the dermis in what are called epidermal ridges. The areas where the dermis projects upward are called dermal papillae. These are required because there are no blood vessels in the epidermis, so all nutrients must be obtained through diffusion from the dermis.
- These ridges are what cause the elaborate patterns in the epidermis of areas with thick skin, such as fingertips.
- There are several cells populating the stratum basale.
- Basal cells, or germinating cells, are large stem cells that undergo continuous mitosis to produce keratinocytes that are being constantly pushed upwards. These keratinocytes replace the skin cells that we shed off every day.
- Melanocytes are the cells that produce melanin, a pigment whose coloration varies from brown to yellow. These melanocytes have processes which extend throughout this layer in order to distribute the melanin.
- Nervous receptors provide information about external stimuli to the brain.
- The spiny layer or stratum spinosum.
- The stratum spinosum is composed of 8 to 10 layers of keratinocytes connected together by desmosomes. Many melanosomes and dendritic cells can be found here. In this layer, keratinocytes produced in the stratum basale divide rapidly.
- The granular layer or stratum granulosum.
- This is where the process of keratinization begins, helping produce keratin that can be found in upper layers.
- Keratinization begins and helps form keratin in upper layers
- As keratinocytes reach the stratum granulosum, they are too far from the dermal capillaries to receive enough nutrients. As a result, they begin to die.
- The clear layer or stratum lucidum.
- The stratum lucidum is only present in thick skin, which can be found at the fingertips, palms, and soles.
- It is a thin, translucent band superficial to the stratum granulosum.
- The corny layer or stratum corneum.
- The stratum corneum is the outermost layer; it is composed of 20 to 30 layers of dead, flattened keratinocytes (essentially just membranous sacs filled with keratin). They are continuously shed and replaced by cells from deeper strata.
- The keratinocytes in this layer are called keratinized cells or cornified cells. They are primarily composed of keratin, which serves to protect the deeper and more vulnerable dermis. These cells are very tightly attached to each other by desmosomes, which are special proteins that join two cells and are very difficult to break. These desmosomes are why one's skin peels off in sheets after a bad sunburn instead of in individual cells.
The Dermis
The dermis, located beneath the epidermis, consists of two layers. About 70% of the dermis is composed of collagen fibers, which give structural toughness and strength. The most superficial layer is the papillary layer while the deepest layer is the reticular layer.
- The papillary layer.
- The papillary layer is named after the dermal papillae. It is composed of loose connective tissue whose purpose is to supply the epidermis with nutrients. It is supplied with capillaries and innervated by nerves.
- The reticular layer.
- The reticular layer is composed of dense irregular connective tissue. It is filled with densely packed elastin fibers, which give the skin its elasticity. This layer is also filled with collagen fibers, which resist that elasticity, in order to keep the skin rigid. One of the major causes of wrinkles is the degradation of collagen fibers due to UV light.
Skin Color
There are three major pigments that influence skin color: carotene—a yellow-orange pigment found in carrots and squashes—melanin—a pigment whose color varies from yellow to brown and is produced by melanocytes—and hemoglobin—a red pigment found in the blood that gives the skin its red tint. Carotene can be synthesized into Vitamin A, which is needed for the maintenance of epithelial cells. Eating large amounts of carotene can also cause the skin of light-skinned individuals to turn orange. Melanin is transferred into the stratum basale and stratum spinosum by intracellular vesicles arising from melanocytes. The two main types of melanin are eumelanin and pheomelanin. Eumelanin is brownish-black and pheomelanin is reddish-yellow. The number of melanocytes is about the same for all races, and there is about one melanocyte in every 10 keratinocytes. In albinism, melanocytes are present but experience interference with melanin production. When exposed to sunlight, melanocytes will gradually increase their production of melanin, peaking at about 10 days after the initial exposure. Freckles appear due to increased melanocyte activity in an area. They occur mostly on surfaces exposed it the sun, such as the face. Hemoglobin, when oxygenated, is called oxyhemoglobin and is bright red. When deoxygenated, it is called deoxyhemoglobin and is blue-purple. When blood vessels constrict, such as they do in response to fear, the skin turns pale and sometimes blue. When the former happens, the condition is called pallor, or paling. When the latter happens, the condition is called cyanosis. When blood vessels dilate, such as they do in response to embarrassment, the skin turns red. This condition is called erythema, erythematosus, or blushing. Vitiligo is a condition in which an individual loses their skin color because their melanocytes stop producing melanin or their melanocytes die. This condition is only cosmetic. UV radiation, while beneficial in small amounts, can cause serious damage in large doses. Melanin protects the body by absorbing the UV rays, and it clusters around the nuclei of epidermal cells to protect the DNA. Unfortunately, melanin cannot protect us from all UV radiation as it is not perfect. Long periods of exposure can cause premature wrinkling and skin cancer even in dark-skinned individuals. A minimum of 15 SPF is recommended in sunscreen, and for fair-skinned individuals, it is better to have a 20-30 SPF sunscreen. Lentigos, or liver spots, are small brown or black spots on the body and are common in older people. They contain abnormal melanocytes and are similar to freckles. They usually occur on sun-exposed skin. One of the main functions of the integumentary system is the synthesis of Vitamin D3 from a cholesterol-based steroid, which is required for the uptake of calcium into our bones. This function is carried out by the stratum basale and stratum spinosum. A low amount of UV radiation is required for this process.
Hair
Hair is comprised of keratin, and hair follicles develop before birth. If the hair shaft is flat and ribbonlike in cross-section, the hair is kinky; if it is oval, the hair is silky and wavy; if it is round, the hair is straight and coarse. The three main types of body hair are terminal hair, lanugo, and vellus hair. Terminal hairs are thick, coarse hairs that grow during puberty. Vellus hairs are short, fine downy hairs found all over the body except for the palms of the hands and soles of the feet. It is thinner than lanugo. This is the body hair of children and adult females.

The lanugo coat is a coat of very fine, soft hairs often found on infants. If lanugo grows on the body of an adult, it is typically a sign of anorexia nervosa. The hair follicle folds down from the surface of the epidermis into the dermis, and sometimes the hypodermis. The deep end of the hair follicle expands to form the hair bulb. A hair follicle receptor or root hair plexus wraps around the hair bulb of each follicle. When the hair is bent, these receptors are stimulated. A hair papilla is a small bit of dermal tissue that protrudes into the hair bulb, containing capillaries that supply nutrients to the hair follicle. The outer wall of the hair follicle is composed of a peripheral connective tissue sheath, or fibrous sheath. In the middle is the glassy membrane, a thickened basal lamina. On the inside is the epithelial root sheath, which is composed of an external and internal part. The region of the hair bulb that produces new hair is the hair matrix. The cells in the hair matrix originate from the hair bulge, slightly above the hair bulb. When chemical signals reach the hair bulge, cells migrate toward the papilla and begin to divide; this is how hair cells are produced. A bundle of smooth muscle called an arrector pilus is attached to each hair follicle. When it contracts, the hair follicle is pulled upright and the skin is dimpled, producing goosebumps. Hair grows roughly 2.5 mm every week. Each follicle goes through its own growth cycle. The active growth phase, anagen, lasts for weeks to years. Following this is the regressive phase, catagen, in which blood supply is cut off from each hair follicle for about 2 weeks. Next is the resting phase, telogen, in which the hair follicle rests for 1 to 3 months. Some people consider there to be an extension of the resting phase, exogen, in which dead hairs are shed and new hairs begin to grow again. The hair follicles on the scalp have anagen phases lasting several years, while the hair follicles on the eyebrows have anagen phases lasting only three to four months at a time; this explains why scalp hairs are significantly longer than the eyebrows.
Nails
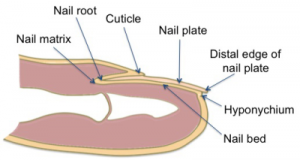
Nails are made of tightly packed keratin. The nails help us grip things with our fingers.
Each nail has a free edge, also known as a nail plate, as well as a proximal root. The deeper layers of the epidermis extend beneath the nail to form the nail bed. The thickened portion of the nail bed is the nail matrix, which is responsible for nail growth. As nail cells are produced in the matrix, they keratinize and slide distally over the nail bed. Nails are mostly pink because of the capillaries supplying the nail bed. The white crescent that lies over the nail matrix is the lunula. The borders of the nails are overlapped by skin folds, called nail folds. The eponychium, or cuticle, is the projection of the proximal nail fold onto the nail body. Below the free edge is the hyponychium, which is where dirt and debris accumulate.
Glands
The two main types of glands in the integumentary system are sebaceous glands, which produce oil, and sudoriferous glands, which produce sweat. There are more sebaceous glands and less sudoriferous glands in thin skin. In thick skin, there are more sudoriferous glands and less sebaceous glands.
Sebaceous Glands
Sebaceous glands secrete sebum, an oily substance that lubricates hair and skin. Sebaceous glands are present everywhere except for areas with thick skin, i.e. the palms of the hands and soles of the feet. Sebaceous glands are located in the dermis layer and are generally connected to hair follicles, except for in hairless areas such as the eyelids. Acne is caused by the inflammation of sebaceous gland ducts.
Sudoriferous Glands
Sudoriferous glands secrete sweat. Sudoriferous glands are found mostly on areas of thick skin. There are two types of sudoriferous glands: apocrine and eccrine.
Apocrine Sweat Glands
Apocrine sweat glands develop during puberty. These glands are located in the ear canal, around the eyes and nose, under the arms, on the areola of the breasts, and in the pubic regions. Mammary glands are one type of modified apocrine gland. Earwax, or cerumen, is secreted by ceruminous glands, the other type of modified apocrine gland. The appearance of cerumen can differ depending on genetic factors. Typical apocrine glands secrete sweat.
Eccrine Sweat Glands
Eccrine sweat glands are found everywhere except thick skin. Eccrine glands are present at birth and continue to secrete sweat from then on. The sweat secretion produced by eccrine glands is made of water and sodium chloride.
Membranes
- Serous membranes line body cavities that have no opening to the outside. They secrete a watery fluid called serous fluid that lubricates surfaces.
- Mucous membranes line cavities and tubes that open to the outside.
- Synovial membranes form the inner lining of joint cavities. They secretes a thick fluid called synovial fluid.
- The cutaneous membrane is the skin.
Homeostatic Imbalances
Burns
Burns are disorders of the integument caused by exposure to intense heat, radiation, electricity, or friction. Burn appearance and treatment varies greatly depending on how deeply the skin was burned. Burns are classified as first, second, and third-degree burns depending on the damage inflicted by the burn. The surface area affected by a burn is calculated using the rule of nines in a typical adult. When the patient is obese, the rule of fives is used. When the patient is an infant, the rule of eights is used.
First Degree Burns
First-degree burns are the most superficial. First degree burns affect the epidermis to the papillary layer of the dermis. First degree burns give the skin a dry red appearance, sometimes with small white blisters.
Second Degree Burns
Second-degree burns destroy most or all of the epidermis, and involve all layers of the dermis. Second-degree burns are pink or red, and cause the involved skin to look shiny and wet. The sensation in tissue with a second-degree burn is weakened.
Third Degree Burns
Third-degree burns involve all of the layers of the skin. Third-degree burns permanently damage tissue. These burns have a charred black or brown appearance. The tissue involved in a third-degree burn often must be replaced using skin grafting.
Allergies and Allergens
An allergen is an antigen that produces a rapid response from the immune system when introduced to the skin.
Infections
An infection is an invasion of dermal tissue by disease-causing agents.
Dermatitis
Dermatitis is an inflammation of the skin due to a variety of factors.
Eczema
Eczema refers to any condition in which the skin becomes itchy or inflamed, but it is most often used to refer to atopic dermatitis. This condition typically begins in infancy or childhood and the skin becomes dry, flaky, and irritated near creases in the skin. Areas include the elbows, the knees, and at the back of the neck. The disorder is likely hereditary. Hot, cold, or dry conditions, as well as stress and certain allergens, can exacerbate eczema symptoms.
Treatment involves preventing infection and soothing itching or discomfort.
Contact Dermatitis
Contact dermatitis produces red, burning, itching, or stinging rashes in response to allergens or other topical irritants. Common causes include poison ivy or heavy metals.
Seborrheic Dermatitis
Seborrheic dermatitis (known as cradle cap in infants) produces scaly patches, dandruff, and incessant itching.
Psoriasis
Psoriasis is a condition resulting in red, flaky patches on the skin. There are five primary types: plaque, guttate, inverse, pustular, and erythrodermic. Psoriatic arthritis can also be considered a variation of this disorder. Many cases of psoriasis are hereditary, but other risk factors include weight or obesity, smoking, medications, infections, alcohol consumption, vitamin D deficiency, and stress.
Plaque Psoriasis
The most common type of psoriasis, plaque psoriasis appears as raised, red, scaly patches on the skin. These scales have well-defined edges and are most often found on the outsides of knees and elbows, the scalp, the lower back, the face, and the palms of the hands and soles of the feet. Topical creams and ointments with and without steroids (i.e. calcipotriene) are the main method of treatment for plaque psoriasis, but it can also be treated by medications or ultraviolet phototherapy.
Guttate Psoriasis
Rather than large scales, guttate psoriasis manifests as tiny lesions or teardrops on the skin. They mainly appear on the abdomen and upper extremities, and they do not appear on the palms or soles like other forms of the disorder. This form of psoriasis is most common in young adults or children, and less than a third of psoriasis patients have it. Dry air is a catalyst in flareups, especially in winter. Severity is determined by the amount of coverage: mild is approximately 3 percent, moderate is 3 to 10 percent, and severe is more than 10 percent coverage or adversely impacts the patient's livelihood and appearance.
Inverse Psoriasis
Also known as flexural or intertriginous psoriasis, intertriginous psoriasis manifests on "flexor surfaces" or in skin folds. Common sites of inverse psoriasis include the navel, groin folds or genitalia, the lips, the ears, the axillae (armpit region), under the breasts (inframammary folds), and between the buttocks (intergluteal cleft). Because these red patches occur in sensitive areas, patients may experience bleeding, pain, or irritation at the sites. They may also experience discomfort and fungal or bacterial infections. Many inverse psoriasis patients have another comorbid form of psoriasis.
Pustular Psoriasis
As the name suggests, raised bumps filled with pus (pustules) accompany the telltale psoriatic scales. Pustular psoriasis is uncommon and can have acute flareups associated with fever or manifest chronically. Other skin disorders can be considered variations of pustular psoriasis, such as pregnancy-associated impetigo herpetiformis.
Erythrodermic Psoriasis
Erythrodermic psoriasis is described as aggressive and is considered the most severe form of psoriasis. It involves a full body rash that can spread quickly from the initial site of inflammation. The rash peels and itches or burns intensely.
Psoriatic Arthritis
Arthritis is an inflammation of the joints, and psoriatic arthritis involves scaly rashes along with joint stiffness and pain. Sometimes joint problems can start before the first rash appears.
Skin Cancer
Skin cancer is the most common type of cancer in the US. The three major types of skin cancer are basal cell carcinoma, squamous cell carcinoma, and melanoma. Skin cancer occurs when the DNA of epithelial cells is damaged, causing the cells to grow out of control. The most common cause of skin cancer is excessive exposure to sunlight.
Basal Cell Carcinoma
Basal cell carcinoma is the most common type of skin cancer. It is curable if found early, especially because it rarely metastasizes (spreads to other organs). BCCs look like smooth, pearly bumps which are mostly found on the face, neck, and back.
Squamous Cell Carcinoma
Squamous cell carcinoma occurs on parts exposed to the sun. SCC often develops on areas with actinic keratoses, which are crusty red sores caused by UV exposure. SCC looks like firm red bumps susceptible to bleeding and crusting.
Melanoma
Melanoma is deadly if not found early because it metastasizes quickly. It is most common in the southern hemisphere where the ozone layer is thin. Melanoma looks like irregular dark spots with a different appearance than a patient's moles.
ABCD Test
You can separate skin cancer with other skin disorders by using the ABCD of skin cancers.
- Asymmetry- the area is not symmetrical
- Borders- the borders are not even
- Color- different shades and varieties can signal skin cancer
- Diameter- if the diameter is larger than 1/4 inch or 6 mm, it is likely it is melanoma.